Recovery exists along a spectrum, with about 7/8% being mostly recovered. The good news is that some people have recovered! I’d love to see the recovery figures higher. One possible reason why that isn’t happening is because…
Most of the information out there is unreliable
The most cited science researcher in the world is John Ioannidis, who has published extensively on Why most published research findings are false. He has over half a million citations.
As far as Long COVID goes, he’s right. Many of the published papers on ‘effective’ Long COVID treatment are unreliable. I maintain a list of supposedly effective treatments at LongHaulWiki.com. Of the 5 randomized controlled trials (RCTs), only the HBOT study is consistent with the survey data I gathered in the Patient Experiences Survey. One of the RCTs failed to disclose financial ties between the researcher and the company making the phytochemical product the researcher studied.
Long story short, the chronic illness space is full of unreliable information. Unfortunately, it takes some time and effort to teach yourself science and medicine to figure out what’s unreliable. If you are willing to put in the work, see this post explaining good versus bad survey research. If you don’t have the time, here are some pointers:
- Financial conflicts of interest often cause information to be unreliable. Researchers need to get research funding, so they may manipulate their results into something sexy. Medical professionals need to make a living, so they may downplay harms caused to their patients and overstate their results. They may receive kickbacks or referral commissions on treatments they recommend. Some patients make money on the treatments they promote. Patient ‘advocacy’ groups often need funding to survive.
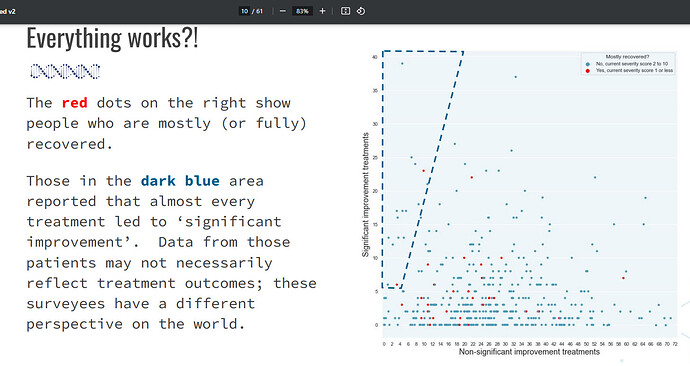
- Some patients report their outcomes in weird or unintuitive ways. Their definition of ‘brain fog’ may be different than other people’s. They may have a ‘everything works’ bias, sometimes caused by them starting a long list of treatments at the same time.
Recovery and the microbes that live inside us
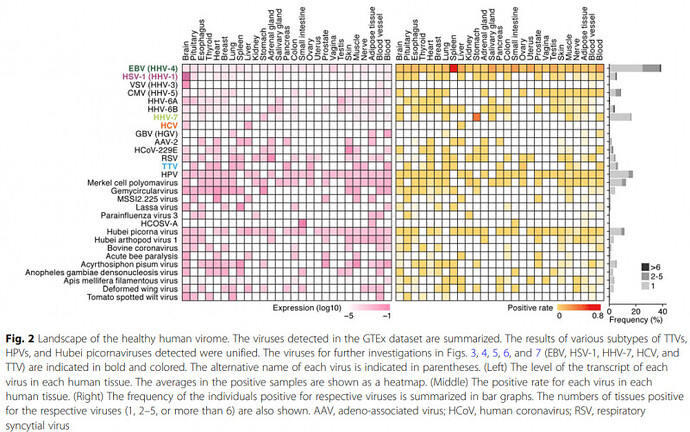
While many doctors erroneously believe that the body is sterile, microbiologists know that all sorts of microbes live inside our tissues. Viruses, bacteria, and fungi live inside our nerves, brain, organs, etc.
https://doi.org/10.1186/s12915-020-00785-5
Changes to the ecosystem of these microbes may be driving Long COVID and related syndromes. Whether or not this theory is true doesn’t affect treatment much; however, it can be a useful memory tool for memorizing some nuances of treatment.
You can think of recovery as treating an unknown infection. You can try interventions one at a time to push the human microbiome around. Eliminating or suppressing one species will affect the entire ecosystem because:
- Microbes can behave synergistically with one another and engage in ‘teamwork’, e.g. the HIV virus helps other microbes kill its host because HIV weakens the immune system.
- Microbes often compete with or interfere with each other, e.g. malaria (specifically Plasmodium vivax) causes fevers that can wipe out a Syphilis infection. The Nobel prize for medicine was given out for this discovery.
Sometimes an antimicrobial treatment will help symptoms, possibly because it makes the environment less favorable for a problematic infection. Sometimes it will make things worse, possibly because it is hurting a microbe that is keeping the problematic microbe in check. Oftentimes it will not make a meaningful difference. These are the patterns that survey data is revealing.
In practice, what we know is:
- There is no testing that can predict a treatment’s outcome. It would be great if this testing were to exist, but we haven’t figured it out yet.
- Effective treatments seem to be a double-edged sword as they will cause harm in some people.
So, patients can:
- Start with low dosages before moving up to higher dosages.
- Discontinue early if it looks like treatment is going the wrong way.
Some top treatments for recovery
- High pressure HBOT - see the primer for some safety information that the clinics won’t tell you about. This is the most proven treatment.
- Extended fasting (primer)
- Black seed oil ?
- *Appeared as a top treatment in the Treatment Outcomes survey but not the newer Patient Experiences Survey.
- Cat’s claw ?
- Nattokinase, serrapeptase ?
- NAC???
- Various prescription antimicrobials listed here, e.g. statins. Colchicine is not listed.
Important caveats
The list above list is derived from survey data, which may be unreliable and generate false signals.
These treatments carry risk. For all of these treatments, some patients report negative experiences.
While the prescription drugs are important, I gloss over them because it’s an advanced topic, they have safety issues, they’re harder to get, and most people won’t try them. I apologize for glossing over this important topic because many of the top treatments fall in that category. You sort of have to be your own doctor if you decide to try them.
Treatments for symptom relief
In general, these treatments don’t do much other than slapping a bandaid on the problem. There is no effective bandaid for many symptoms.
- Pacing strategies (primer) - very safe.
- Low histamine diet (primer) - very safe, likely more effective in patients with food intolerances.
- Gluten free diets (primer) may also be worth trying, e.g. if a low histamine diet fails.
- For POTS, some of the first-line treatments mentioned by Bisaccia and colleagues are very safe (though they may not do much). Specifically:
- liberal intake of water and salt
- drinking water before getting up in the morning
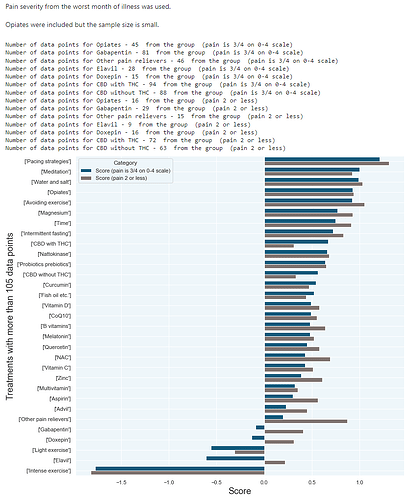
For pain reduction: gabapentin appears to be worse than treatments that do nothing or have a placebo effect. Meditation, etc. may be far more prudent than gabapentin. Opiates also have high patient satisfaction (on average); however their problems are well known.
Has anybody tried ___? Here's how you can get answers to that question fast
Antihistamines have been suggested for histamine intolerance and MCAS. See this thread for a deeper dive.
We need to take safety more seriously
In support groups, there aren’t a lot of people posting negative anecdotes for various reasons:
- You will often get attacked for saying something negative about a treatment.
- It doesn’t get clicks, views, upvotes, etc.
- Many platforms and support groups will actively censor information about interventions that are highly politicized. This can silence negative anecdotes.
This creates blind spots because there isn’t enough attention about treatments going wrong. Social media platforms make this problem worse because their algorithms will push popular content (e.g. recovery stories) over unpopular content about treatments going badly.
Clinicians have this problem but in a different way. Because most of them need to make a living by selling their medical services (or they’re chasing clout), they have an incentive to downplay bad treatment reactions as “detox” or “Herx” reactions. This is DANGEROUS behaviour and I strongly encourage patients to become better informed.
Patients need to be aware of systemic problems in the mainstream and alternative/uninsured healthcare ecosystems. We don’t have systems tracking treatments that go wrong. We don’t have great data as to why Heidi Ferrer and Jack committed suicide following treatments that went badly. Heidi Ferrer worsened following COVID vaccination which led her to mess around with Ambien (known to lead to suicide). What really caused her messy suicide? I don’t know. Jack was a ME/CFS patient who I believe worsened after HELP apheresis.
Nonetheless, many medical ‘professionals’ continue to operate without adequate monitoring of whether they’re causing more harm than good. We don’t have good oversight of the HELP apheresis clinics. Nor do we have good oversight of SSRIs, gabapentin, psych drugs, and antibiotics- all drugs that rank poorly when surveys measure patient satisfaction among chronic illness sufferers.
So please… I implore you to take patient safety more seriously. Mainstream medicine, alternative medicine, and support groups all have problematic blind spots. It is possible that harmful treatments and protocols push patients away from recovery. However, there is very little reliable data as to whether or not that is happening.
Tests that come back positive
While test results for Long COVID are often similar to healthy patients, there are a few tests that are more likely to come back positive.
Long COVID and post-vax patients are more likely to be diagnosed with thyroid disorders and autoimmune diseases. This is according to the Risk Factors survey; PLRC survey data has somewhat similar results (see slide 86).
Diagnosing thyroid disorders:
- Some clinicians believe in subclinical (borderline) thyroid disorders while others don’t. You can look at your own lab results to see if you are in the subclinical range.
- There are additional tests that can be run at the clinician’s discretion such as auto-antibody tests (e.g. anti-TPO).
Diagnosing autoimmune conditions:
- PCPs and family doctors often miss autoimmune conditions because the symptoms are non-specific (could be caused by many different conditions) and because they don’t specialize in autoimmune conditions.
- There is often a subjective element to the diagnosis. Clinicians may also be biased if they don’t believe that their patient is ill, e.g. because of what’s in the patient’s medical records like anxiety, FND, etc.
- If enough auto-antibody tests are performed, false positives are far more likely to occur.
Please note: Doctor shopping and other behaviors can increase your chances of receiving a diagnosis. Is that good medicine? Probably not. However, some patients may want a diagnosis for non-medical reasons such as qualifying for disability, being taken more seriously, etc.
Other testing notes:
- ME/CFS patients are more likely to have POTS. Long COVID is probably similar. There is an at-home version of this. The Health Rising ME/CFS website has an analysis of the NASA Lean test along with simple instructions for performing the test in a doctor’s office. While the guide suggests stopping certain medications, please note that discontinuing many anti-depressants (e.g. TCAs, SNRIs) can be very dangerous and sudden withdrawal is often the most dangerous way of stopping those medications.
- Pulse - You can measure your own pulse to see if it is too fast (e.g. over 100bpm while resting), too slow (below 60bpm is borderline slow for non-athletic adults), or irregular.
- Abnormal sweating → QSART
- Damage to the small fibers of the peripheral nervous system can cause burning pain, numbness, inability to sense hot/cold, and/or tingling sensations. A skin biopsy can measure the density of nerve fibres in the skin and test for small fiber neuropathy.
- Sleeping patterns - consumer smartwatches and fitness trackers can sometimes pick up abnormal sleep.
You can also ask your doctor to put in extra effort to look for other potential causes of your health problems (differential diagnosis). You may have a known health condition that is not Long COVID, ME/CFS, etc. You can refer to Tables 2 and 3 in this published paper regarding differential diagnosis of ME/CFS.
Questionable positive test results
Some practitioners in the alternative space will sometimes recommend non-conventional testing. One potential problem with this is that the tests can come back “positive”, which helps the practitioner financially since they’ve validated the patient (“proving” that the patient is sick) and the doctors can then proceed to “treat” the patient for Lyme, microclots, etc.
Lyme and tickborne infections: Lyme infections are real. However, the reality is that testing is not good. The conventional tests often miss Lyme infections. The non-conventional tests have problems with false positives, false negatives, or both. Be careful about false positives.
If the conventional test is negative, often the only way to know if you have it is to try treatment. However, be careful because Long COVID patients often react very negatively to antibiotics in ways that healthy patients don’t. Safer Lyme treatments may include Plaquenil, oil of oregano (contains carvacrol), essential oils, Biocidin, black seed oil (contains carvacrol), cinnamon essential oil, monolaurin, HBOT, methylene blue.
Microclots: Some healthy patients have them, some Long COVID patients do NOT have them. (See Caroline Dalton’s presentation dissected in this post.) However, some practitioners will end up giving positive test results for almost all their patients because their subjective interpretation magically lines up with their financial incentives. ![]()
Risks related to testing
The following tests may be worth doing but please educate yourself about the risks.
- Lumbar puncture, which can cause CSF leaks. CSF leaks may be more likely in patients with hypermobility (?).
- MRI with contrast / gadolinium contrast dye → gadolinium toxicity
Do not suddenly discontinue psych meds, SSRIs, or benzos prior to POTS testing or allergy testing. The labels (or product monographs) for these drugs often recommend against sudden discontinuation. The labels are different between Canada and US.
Some supplements and alternative treatments that are much riskier than you think
- Ashwaganda - PSSD risk (some PSSD sufferers commit suicide)
- Lion’s mane
- Acupuncture (!) - see this post regarding some bad experiences. It does not seem to be anywhere as devastating as PSSD.
Regarding supplements: a few are basically prescription drugs, e.g. red yeast rice (lovastatin) and kratom (opiate effect).
Recovery story compilations
These are sources of data but there is some degree of unreliability to them.
Survey data
Watch the video below or use the slides (slides are in the video description). The video and slides explain some ways in which survey data is unreliable.
r/LongHaulersRecovery has:
- An index of recovery stories here
- A ChatGPT summary of 60 recovery stories from different subreddits.
In general, I am suspicious of this data because most of the recovery stories in the ChatGPT summary post mention some type of exercise, which is often not graded exercise therapy (note: ChatGPT does miscategorize treatments).
Survey data strongly indicates that exercise is harmful for most patients. It is unclear if there is a small subset of patients that benefit from exercise (mainly in those with low severity). Maybe it’s happening, maybe it’s not. We need something better than survey data to really know the answer because the responder rate for exercise is so low. However, I doubt that we will get reliable research on this topic.
Youtube
Youtube has various recovery stories, with some channels hosting a large number of recovery stories. I have a list of such Youtube videos here; you’ll have to click on the channel name for all of the recovery stories on a particular channel.
A problem that affects many Youtube channels is that the Youtuber is trying to sell something- such as a course or brain retraining program.
- CFS Health seems to be buying views.
- Rachael Elizabeth doesn’t always disclose her affiliate marketing relationship(s).
So, I trust these stories even less than r/LongHaulersRecovery because that subreddit isn’t trying to sell stuff.
Popular theories that didn’t pan out
- Microclots - for a deep dive into why the science is bad, see this post.
- Bruce Patterson / IncellDX - the statins seem to work for some people, but other interventions like maraviroc and cytokine testing seem to be a bust.
- Paxlovid - The Stanford RCT was scrapped, and PES survey data suggests that this is a flop.
- Spike protein detox - see PES survey data
- Nicotine / nicotinic receptors theory - see PES survey data
- IVIG / immunomodulators - see PES survey data, and this post about the study’s patients speaking out about Avindra Nath’s data
Probably doesn’t work but the data is less definitive:
- Corticosteroids / autoimmunity suppression - see the discussion in the PES survey data video.
Alterative treatments
Most of them have been tried by many people and don’t seem to lead to recovery. That includes homeopathy, osteopathy, chiropractors, most but not all supplements, etc.
To find data on popular treatments, see the thread below. If the treatment is popular and doesn’t seem to work, you can save time and money by trying more promising treatments. Also, some treatments seem to be far riskier than you would expect (e.g. acupuncture).
Heavy overlap between Long COVID, ME/CFS, and post vax
Survey data suggests that the symptoms of these three conditions overlap heavily.
In practice, we have trouble spotting any differences between these three groups because a different phenomenon overshadows any medical differences. Specifically, patients answer surveys in unintuitive ways. How data is gathered will affect the data and create different groups of patients based on how they answer questions. Some patients will overreport symptoms relative to other patients. Some patients have a ‘everything works’ bias when it comes to reporting treatment outcomes.
https://sickandabandoned.com/wp-content/uploads/2024/01/2024-01-07-pes-slides.pdf
Clinicians currently aren’t very sophisticated when it comes to assessing the reliability of patient-reported symptoms and outcomes. This can result in misdiagnosis. It can result in clinicians developing misconceptions about the effectiveness of their medical advice. People tend to be overly optimistic about what their treatments are doing.
We need to work on the miscommunication problems first before we think about whether or not there are subtle differences between Long COVID and ME/CFS.
Using ME/CFS knowledge for Long COVID (and vice versa)
Some things we know about ME/CFS:
- Rituximab doesn’t work for ME/CFS. see https://doi.org/10.7326/M18-1451
- Cytokine panel testing doesn’t work for ME/CFS
- The CPET test can be used to diagnose PEM in ME/CFS patients so that they can get disability assistance. (Long COVID patients often qualify for a ME/CFS diagnosis.) See Slide 12 https://batemanhornecenter.org/wp-content/uploads/filebase/providers/PEM-Lecture-Slides-ECHO-v4-5_17_2022.pdf
Experimental treatments
Patients have gotten their hands on the following treatments so limited data is available on those treatments:
- BC007 (anecdotes)
- Remdesivir’s metabolite (GS-44)
- Sofosbuvir (search Reddit)
- Truvada / tenofovir - see the slides for this video
Recap
There is some scientific uncertainty as to whether or not we already have treatments that lead to recovery. (While people have recovered, it may not necessarily be due to treatments that they tried.)
If you believe that treatments are leading to recovery in some people, then refer to the “Top treatments” section.
If you don’t believe that any treatment leads to recovery, then there are still some ‘bandaid’ treatments worth doing such as pacing strategies. Some of them are very safe (e.g. pacing, meditation). Refer to the earlier section “Treatments for symptom relief”.
I hope this helps. ![]()