Summary:
- Both the Stanford and Yale trials on Pax for Long COVID were rigged by making the control group take ritonavir and to experience side drug side effects that they wouldn’t otherwise experience. The Stanford trial was halted anyways.
- Paxlovid is definitely not a silver bullet for Long COVID. If Paxlovid helps, it is likely less attractive than HBOT in terms of efficacy (though high-ATA HBOT is quite expensive).
- There are serious drug interactions associated with Paxlovid. Some of the professional medical advice out there may be dangerously wrong; please watch out for the conflicting advice out there.
Drug interactions
Paxlovid contains ritonavir, a HIV drug that’s intentionally added so that your body takes longer to metabolize the other drug (nirmatrelvir). Ritonavir has the same effect on many other common drugs. It can cause them to build up in your body, potentially causing an overdose.
Some medical professionals may recommend that you stop certain drugs cold turkey while taking Paxlovid. That can also be very dangerous and goes against the recommendations on the FDA label and/or product monograph.
Pfizer and its research collaborators also seem to anticipate a possible interaction between Paxlovid and vaccinations (COVID and non-COVID) based on who they are excluding from their Paxlovid for Long COVID trials. I find this to be weird but their actions speak for themselves.
For those of you buying Paxlovid without a prescription, please get the right medical oversight.
Ontario Science Table recommendations (*may be dangerous, contradicts FDA and Canadian drug labels)
A government-funded group in Ontario Canada put out a guide on prescribing Paxlovid. Skip to page 3 for a giant list of common medications. It recommends that many benzodiazepines be stopped (‘held’) while taking Paxlovid and restarted 2 days after the course of Paxlovid is finished.
The problem is that stopping benzodiazepines cold turkey can be dangerous. The Canada product monographs are stronger than the American FDA labels in warning about the dangers of suddenly stopping benzodiazepines. The alprazolam (Xanax) product monograph states that benzodiazepines (like Xanax) can “produce severe or life-threatening withdrawal symptoms.” It gives a warning: “Avoid abrupt discontinuation or rapid dose reduction of XANAX and XANAX TS.”
The Ontario Science Table has the opposite opinion and the authors don’t seem to have read the Canadian product monographs for benzodiazepines. They seem to believe that it is ok to abruptly stop benzodiazepines. Hence they are ok with recommending the following for alprazolam: “Hold and restart 2 days after completing nirmatrelvir/ritonavir.”
They can’t all be right. Either it’s safe to suddenly stop benzodiazepines or it isn’t. The takeaway here is that not all medical professionals are right. Some of them will give you dangerous advice.
*Note: the Ontario Science Table website was dissolved on September 6 2022. Its information is no longer being updated.
Finding competent advice
I don’t know.
You could give yourself a crash course in pharmacokinetics and learn about the core concepts such as half-life, AUC, etc. Then you could read the 40+ page FDA label for Paxlovid.
The finer details
If a drug is an inhibitor, it will reduce/inhibit the action of certain enzymes that break down drugs. This can increase the concentration of drugs that are mainly cleared from the body through those particular enzymes. If multiple enzymes are involved in breaking down a drug, then an inhibition of only one of those enzymes may not matter much. You can usually search Google scholar (or Google) to find scientific papers about particular drug interactions and what the researchers are seeing in real-world patients. (Sometimes the papers are conflicting so you may want to read more than one.)
If a drug is an inducer, it will increase the activity of enzymes that break down drugs. This will lower the concentration of a drug in the body. This can also be a problem because it can make drugs less effective or maybe create withdrawal problems. The inducer effect can take days to ramp up to its full strength.
If a drug is a substrate of an enzyme or transporter protein, it means that the enzyme or transporter will act on that drug.
Here’s a summary of some of the finer details for Paxlovid (Nirmatrelvir/ritonavir). While most of the concern is over the drug being a strong inhibitor of CYP3A4, the drug is also a strong inhibitor of CYP2C8. The CYP2C8 enzyme is implicated in fewer drug interactions so that may be why it isn’t discussed as much.
| Metabolic Pathways | |||
|---|---|---|---|
| Inhibitor | Inducer | Substrate | |
| CYP1A2 | ++ | ++ | + |
| CYP2A6 | ++ | ++ | |
| CYP2B6 | ++ | + | |
| CYP2C19 | + | + | ++ |
| CYP2C8 | +++ | ||
| CYP2C9 | + | + | ++ |
| CYP2D6 | ++ | + | |
| CYP2E1 | + | ++ | |
| CYP3A4 | +++ | +++ | |
| UGT1A1 | ++ |
| Transporters | |||
|---|---|---|---|
| Inhibitor | Inducer | Substrate | |
| OATP1B1 | ++ | ||
| OATP1B3 | ++ | ||
| OCT1 | ++ | ||
| P-gp | ++ | ++ |
If the transporters are (strongly) inhibited, then there can be a build-up of the drug in particular cell types or in certain parts of the body. Transporters that would normally flush the drug out no longer do what they would normally do. That can be a problem, though most people do not have concerns about Paxlovid.
This gets complicated. I don’t really know what’s going on.
Clinical trials on Paxlovid for Long COVID
Pfizer funded 2 studies that are run in conjunction with university researchers.
- The Stanford trial ( NCT05576662) stopped recruitment early. A MedPage Today article states:
Two sources familiar with the STOP-PASC study told MedPage Today that trial enrollment had been halted. One was told by a study coordinator that a preliminary review found “inconclusive evidence” for the primary outcome of the study. Another said their first appointment was canceled just a few days before it was supposed to take place, and they were later told that all future enrollment had been halted.
- Yale is currently recruiting for a similar study on Paxlovid in Long COVID patients (NCT05668091).
The Stanford trial is somewhat concerning because it suggests that Paxlovid does not work for Long COVID. If the drug simply did nothing compared to the ritonavir-only control, then they could have simply finished out the trial. Also the trial design is questionable because the control group should not be taking ritonavir… there’s no good reason for long haulers to randomly take that drug. The researchers are clearly running a trial that is rigged to try to make Paxlovid look good. I am deeply disappointed that they have put profits over patients.
Also note that the trial is designed to exclude many typical Long COVID patients such as people who are taking certain prescription drugs (the ones that interact with ritonavir such as benzos, many SSRIs, etc.). It’s not unusual for Long COVID patients to be on drugs to treat their various health problems.
The Yale study (but not Stanford) excludes those with ME/CFS, mast cell activation disorder or POTS.
The NIH also announced that its RECOVER-VITAL study will look at Paxlovid.
Special considerations
Paxlovid may behave (very) differently if the following apply:
- Impaired kidney function
- Severe liver disease, receiving dialysis or renal impairment (eGFR estimate <60 mL/min/1.73 m2 ) as determined by laboratory testing at screening.
- Pregnant or breastfeeding.
- Current or expected use of any medication dependent on or inducer of CYP3A4
- Current or expected use of supplements or herbs (unless medically necessary) that cannot be temporarily held (period as determined necessary by investigators)
- HIV infection with viral load >50 copies/ml
- Acute medical illness currently or within the past 2 weeks, including COVID-19 infection.
- Immunocompromised, as defined by the CDC
- Any concomitant prior chronic condition that has caused debilitating symptoms, even if episodic, such as myalgic encephalomyelitis/chronic fatigue syndrome, chronic Lyme disease, multiple sclerosis, fibromyalgia, mast cell activation disorder, and small fiber neuropathy, postural orthostatic tachycardia syndrome, lupus erythematosus, and others or any prior condition associated with immune dysfunction.
The list above simply comes from the inclusion and exclusion criteria for the Stanford and Yale trials that are in collaboration with Pfizer. Those criteria also mention:
- Other medical condition(s) or concomitant therapy […], as determined by study investigators
- History of COVID vaccine within 28 days prior to enrollment, or other vaccine (influenza, shingles, etc.) within 14 days of enrollment, or planned use of any vaccine until the primary endpoint has been met (10 weeks)
I have no idea why they think that vaccination would interact with Paxlovid, though we do know that it interacts with Long COVID. The Pfizer COVID vaccine would likely be the most popular COVID vaccine among patients that they enroll. Because they would collect detailed safety information and patient outcome information, maybe they simply wish to avoid gathering data on vaccine injury (and there is no interaction with Paxlovid…?). I don’t know.
The complete lists can be found at NCT05668091 (Yale) and NCT05576662 (Stanford).
Survey data
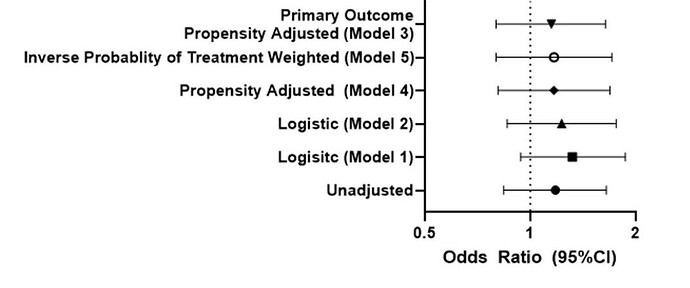
15 people tried Paxlovid (#8) and it lagged slightly behind ivermectin (#6) and HCQ (#5). It also lagged behind HBOT, which is the most proven Long COVID treatment right now.
Has anybody tried ___? Here's how you can get answers to that question fast
Not shown: IVM and HCQ were associated with people recovering while nobody recovered on Paxlovid AND rated the drug highly.
The bottom line
As a treatment for Long COVID, this drug is not the most exciting thing in the world.
- Efficacy: not good if the Stanford trial failed.
- Safety: not good. Survey data shows that its riskiness is above average. (However, this may be skewed by people taking Paxlovid without medical supervsion.)