The most reliable scientific evidence comes from double-blind randomized controlled studies. There have only been a handful of those for Long COVID or similar conditions:
- Hyperbaric oxygen therapy (HBOT)
- Leronlimab, a CCR antagonist
- AXA1125
- Phyto-V (RCT link)
- IVIG for post-polio syndrome (and other conditions), which may be unrelated to Long COVID
- Rituximab for ME/CFS, which should be more like Long COVID than post-polio syndrome
Links to the RCTs can be found at the List of doctors and approaches - Long Haul Wiki
Phyto-V - why I don’t trust the published science on this Phytochemical capsuleOf the RCTs listed above, only 2 of them had positive statistically significant results. I won’t talk about Phyto-V here because it probably needs its own post. The Phyto-V data may be unreliable because Robert Thomas has potential conflicts of interest with keep-healthy.com. So that leaves us with HBOT…
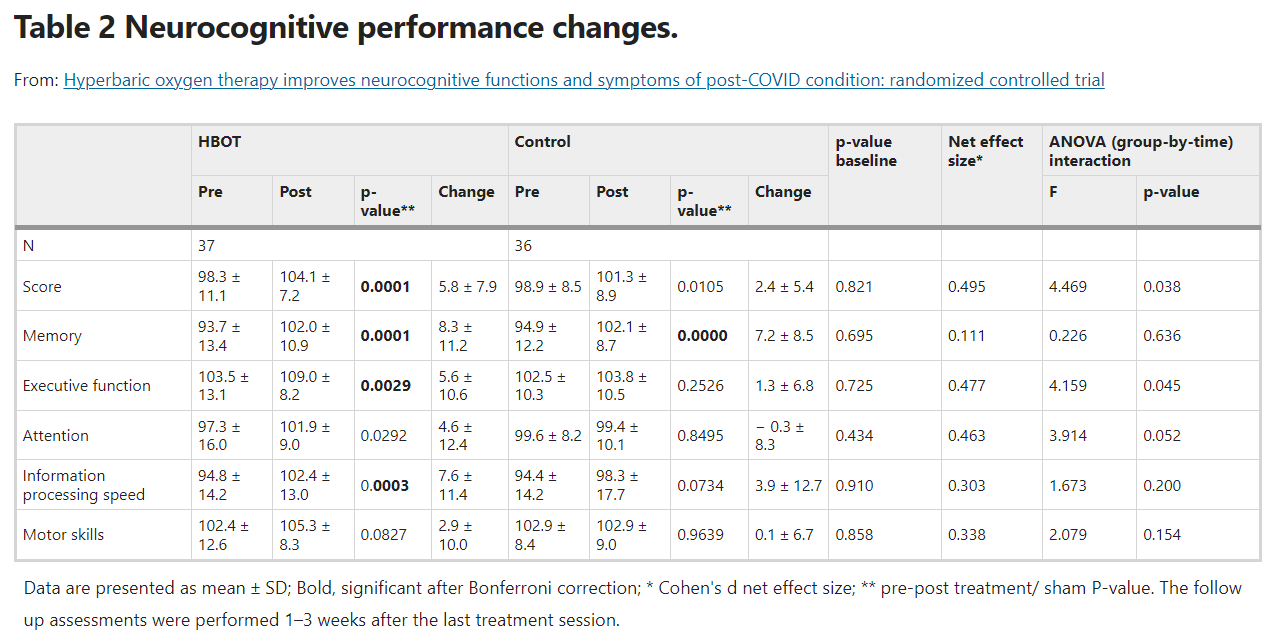
The Shamir Medical Center RCT
Shamir Medical Center in Israel funded a randomized controlled trial of HBOT on Long COVID patients. It compared HBOT at 2ATA (with oxygen) to ‘sham’ HBOT that was as mild as possible to give the impression of HBOT treatment. Both the high-pressure HBOT group and the ‘sham’ control group experienced a few cases of barotrauma. The blinding was fairly good as “the correct group allocation perception rate was 54.1% and 66.7% (p=0.271) in the HBOT and control groups respectively”.
One strength of the trial was that endpoints were pre-registered (NCT04647656) to ensure that the results are reliable and free of data mining. The trial met its primary endpoint of cognitive improvement as measured by Neurotrax, a computerized set of tests that objectively measures cognitive performance.
How to get more information: The study results paper can be found at Hyperbaric oxygen therapy improves neurocognitive functions and symptoms of post-COVID condition: randomized controlled trial | Scientific Reports
Safety considerations with HBOT
For some reason, a few people seem to react very badly to HBOT on the first session or within the first few sessions. This seems to happen even at lower pressures.
One anecdote: Veronica Smith reported worsening after 9 sessions at 1.5 (?and 2?) ATA. Negative symptoms became clearer following dives 4 and 5.
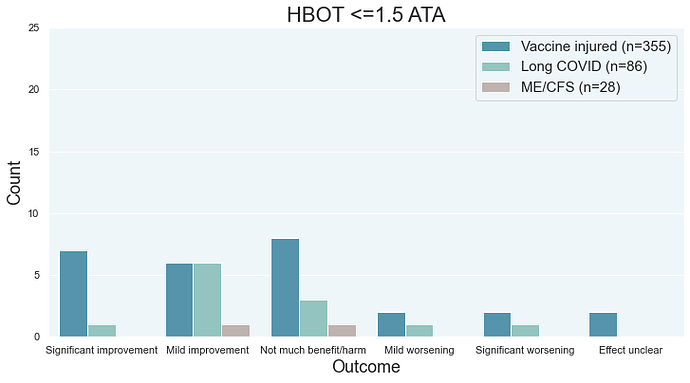
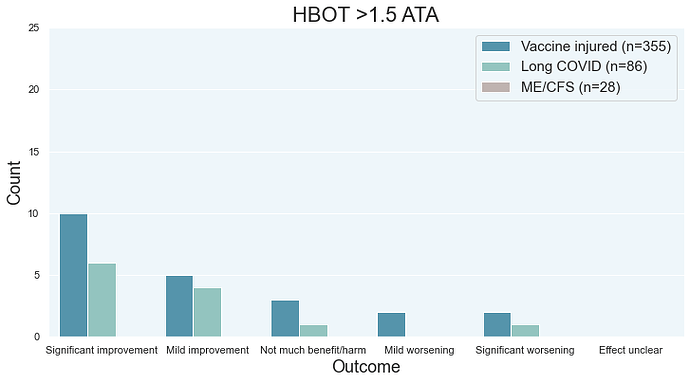
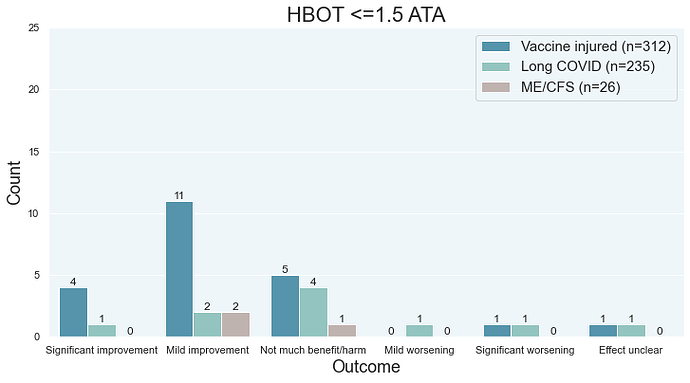
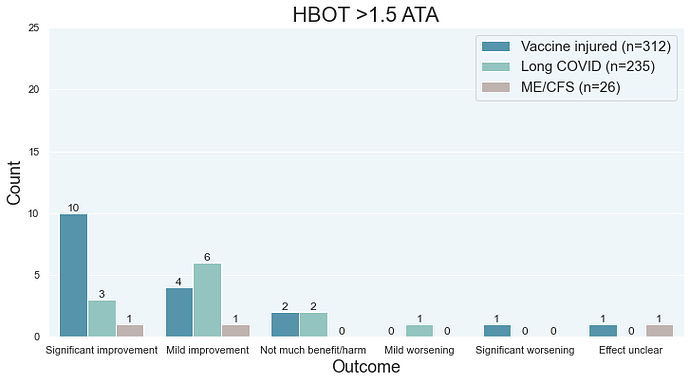
Here’s survey data showing the same idea. The rate of mild and significant worsening is roughly the same between low and high pressure HBOT.
To save some money, you can start with lower pressures to see if you will react and to reduce your exposure to HBOT. Lower pressures = less HBOT. A Swedish study provided ~1.18 ATA HBOT to its sham group, which experience adverse events similar to the treatment group (which got HBOT at much higher pressure).
Oxygen toxicity
An animal study found that excessive HBOT can lead to death in lab animals. See Warren et al. (DOI:10.4049/jimmunol.121.1.315). Human patients also report the same thing. So after 10-40 sessions, you may want to start paying attention to whether or not HBOT is making your symptoms worse rather than better.
Fire hazard
One of the ways to try to save money/time is to buy a soft shell chamber and to sleep in it (so that it doesn’t take “time” to do your HBOT). You would be sleeping in a fire hazard because oxygen and pressure makes fire burn faster.
So… you really need to know what you’re doing if you try something like that.
Herx reactions
If you have Lyme or spirochete bacteria dying off, you may experience serious side effects. However, if you can confirm that a Herx reaction is happening (e.g. previous similar reaction with antibiotics), it may be worthwhile to use HBOT to slowly kill off bacteria under competent medical supervision. Horowitz is a Lyme doctor who explains Herx reactions in this video.
However, be careful about doctors who have a financial incentive to mis-diagnose you with a Herx reaction. There are some bad doctors who will try to hide their mistakes/ignorance/grift by blaming bad outcomes on a “Herx” reaction - see the thread on it.
Cost
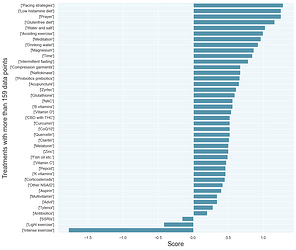
Only a small portion of people seem to really benefit from HBOT- there’s some additional data here in the ‘what worked’ video. If you aren’t noticing results within the first several session of high-pressure HBOT, then you don’t need to throw your money down a pit.
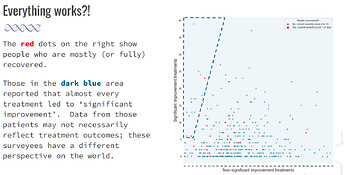
If you scroll up to the charts, you can see that most people don’t report significant improvement. It also turns out that the survey data is optimistically biased so people will report slightly improvement for treatments that may be doing nothing.
High pressure versus low pressure
Unfortunately, the higher pressure HBOT seems to be delivering more benefit than lower pressure HBOT. It is a lot more expensive. Whereas you can spend several thousand dollars to $15K to buy a soft shell chamber, buying a hard shell chamber capable of higher pressures is not so straightforward.
I don’t know if you can make that up by doing a lot of low-pressure HBOT. I just haven’t seen data on that yet.
The UK
The UK has a series of charities that provide HBOT at a lower cost.
The bottom line
While cost will be a barrier for some people, this is the most proven treatment for Long COVID. Hopefully other treatments will have high-quality studies supporting their use so that other treatments involves less guesswork and dice rolling. I certainly don’t think that HBOT is the only treatment you should look at, especially because most people won’t respond to it.