Among Long COVID patients:
- 16.0% had a formal diagnosis before Long COVID.
- 10.0% had a new diagnosis after Long COVID.
Among the post-vaccination long haulers:
- 21.8% had a diagnosis pre-vax.
- 13.9% had a new diagnosis post-vax.
Data from http://sickandabandoned.com/wp-content/uploads/2023/06/SAA-Risk-Factors-Survey-FULL.pdf
![]() Note: The actual rate of new-onset autoimmune disease may be much higher because many people have an undiagnosed autoimmune condition.
Note: The actual rate of new-onset autoimmune disease may be much higher because many people have an undiagnosed autoimmune condition.
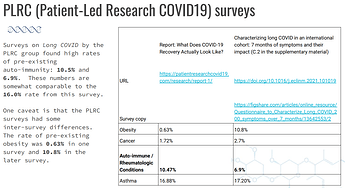
Going back to pre-existing autoimmunity, the PLRC group had similar findings for their 2 surveys. see slide 86 for references.
Diagnosing autoimmune disease is hard
Unfortunately, diagnosis is hard because:
- The symptoms are non-specific; they are often vague and are not specific to a particular autoimmune disease.
- In practice, family doctors / GPs aren’t that good at spotting autoimmune disease or suspecting that it may be a cause.
- For many autoimmune diseases, diagnosis involves subjective components.
A paper by Narain and colleagues looked at differences in diagnosis between their center and the diagnosis from the referring practitioner. The results?
We found a 49% agreement between the referring and final diagnoses (κ = 0.36).
https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/217748
The diagnosis was the same only half the time (!!).
On a practical level, autoimmune disease can also go undiagnosed because it can take months or even a year to get an appointment with a specialist.
Celiac disease
Celac disease has a more clearcut diagnosis than other autoimmune diseases since it has a great biomarker- the biopsy. The biopsy is more reliable than the tests normally used to diagnose most autoimmune diseases:
- Looking at symptoms and response to certain drugs/treatments
- Blood tests for antibodies
- Genetic tests
Because the testing is more reliable, the data for celiac disease can be cleaner than the data for other autoimmune.
A 2003 study by Fasano et al. (DOI:10.1001/archinte.163.3.286) does a deep dive into the topic and strongly suggests that celiac disease is significantly underdiagnosed in the US. It cites a survey of patients:
a recently published survey of 1612 patients with CD in the United States revealed that the average gap between the onset of symptoms and the time CD diagnosis was confirmed was 11 years
The bottom line is that there is a lot of autoimmune disease out there that is undiagnosed.
There are also a few people who would benefit from a gluten-free diet even though they don’t have celiac disease. See the literature on non-celiac gluten sensitivity, e.g. Nutrients | Free Full-Text | Non-Celiac Gluten Sensitivity: The New Frontier of Gluten Related Disorders
Celiac disease and Hashimoto’s in chronic illness patients
While celiac and Hashimoto’s made up 41% (34/82) of pre-existing conditions , they made up 11% (5/46) of new-onset conditions.
It’s not clear to me why they are under-represented in new-onset autoimmunity. It could be the case that there are different types of autoimmunity, so that’s why certain types of autoimmunity are more likely to show up as a new-onset condition in chronic illness patients.
Small fiber neuropathy (SFN)
The rates of SFN seem to be much, much higher in long haulers than the general population… maybe 77 times or higher.
The rate of new SFN (2.3% or 7/298) seems extremely high in Long Haulers. The new-onset rate is 77 times the 52.95 per 100,000 population rate reported by Chan and Smith (DOI:10.1002/mus.25082).
Note: the survey did not specifically ask about SFN and what type of SFN (autoimmune or not); this likely led to under-reporting.
Not all neurologists are experienced in diagnosing SFN, so you may need to shop around to find a specialist who knows about the condition.
Some symptoms of SFN
The symptoms of small fiber sensory neuropathy are primarily sensory in nature and include unusual sensations such as pins-and-needles, pricks, tingling and numbness . Some patients may experience burning pain or coldness and electric shock-like brief painful sensations.
from the Johns Hopkins page - https://www.hopkinsmedicine.org/neurology_neurosurgery/centers_clinics/peripheral_nerve/conditions/small_fiber_sensory_neuropathy.html#:~:text=The%20symptoms%20of%20small%20fiber,shock-like%20brief%20painful%20sensations.
Auto-antibodies
Some people believe that auto-antibodies are a good test for autoimmune conditions. However, the problem is that some healthy people will have the same auto-antibodies. If you do enough testing, you will find something. However, it may not necessarily mean that you have autoimmunity occurring.
The science on this topic is not settled. Somebody like Gerd Wallukat (who is associated with a lab that sells auto-antibody tests) will argue in favour of the auto-antiibody theory. Others have argued against it. For example, Aaron Ring’s lab at Yale has tested for thousands of auto-antibodies; they have found similar levels in Long COVID patients, post-vax myocarditis patients, and healthy controls. For both sides of the debate, see the references at Etiology - Long Haul Wiki.
For people who got the adenovirus vaccines (JnJ, AstraZeneca), see this post on PF4 auto-antibodies causing blood clots.
Conclusion
Unfortunately, it’s hard to get a definitive answer as to whether or not you have an autoimmune condition. (Unless it’s something like celiac disease.) Diagnosis and testing aren’t perfect.
However, autoimmunity is something to think about because it seems to occur at very high rates in long haulers. We don’t even know the exact rates of different autoimmune conditions because there are barriers to getting a diagnosis:
- a psychosomatic diagnosis causing doctors to not take the patient seriously
- delays in diagnosis due to wait times
- in general, the high rates of underdiagnosis
- the shortage of specialists that can diagnose SFN.
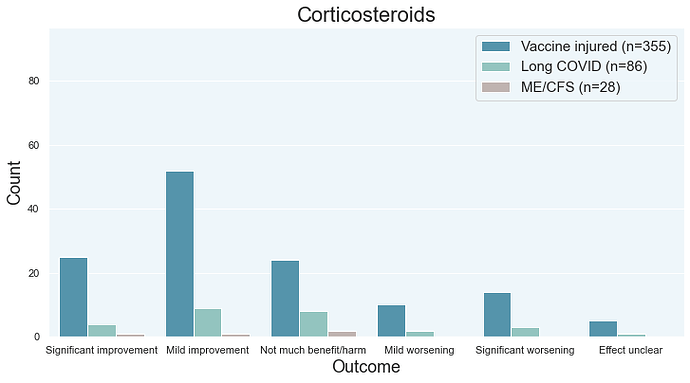
This area of medicine doesn’t have clearcut answer right now. In terms of treatment, the immune suppression approach doesn’t seem to help patients get their lives back by dealing with the root cause (data on recovery here). Corticosteroids, the most popular immune suppression treatment for autoimmunity (and other conditions), can really help some patients feel better and make other patients feel much worse. There are safer, more effective treatments out there.
I wish I had a nice, simple answer for you. But things aren’t very clearcut at the moment. What we do know is that a lot of long haulers have an autoimmune condition and that patients should probably get it checked out.
*Raw data
Raw data to follow in a comment below…