Some researchers like John Chia (who successfully treated his son’s ME/CFS) believe that persistent infections are a major cause of chronic illness. However, it can be difficult to determine the exact infection because current testing is not very good or easy to access. Experimental treatment can involve blindly treating for an infection that may not be there.
This post will go over some key things that we know about treating chronic infections.
Chronic Lyme
Megan Weitner’s 2016 thesis explored the idea of synergy between different antimicrobials. A half dose of drug A plus a half dose of drug B is more powerful than a full dose of either drug A or B. A half-strength attack on two different mechanisms is typically more powerful than a full-strength attack on a single mechanism. The angles of attack include:
- Cell wall disruptor, e.g. cefuroxime, daptomycin
- Membrane permeability or homeostasis mechanisms, e.g. HCQ, fluconazole
- Free radical production, e.g. methylene blue, artemisinin
- Protein synthesis inhibitor, e.g. doxycycline, azithromycin
- DNA transcription, e.g. Rifabutin
Her idea was not new. Combinations of drugs are used to treat tuberculosis and Hep C.
Pulsing is a dosing strategy where the dosing alternates between full strength and no drug being given. This can be helpful in fighting Lyme bacteria as they will switch to a form that makes them vulnerable to antibiotics when antibiotics are briefly stopped.
The concept of chronic Lyme is highly controversial even though research by Monica Embers and others (e.g. Anna Goc) indicate that Lyme bacteria can persist in the body. While the science suggests that chronic Lyme is a real disease, mainstream medicine has yet to embrace those ideas for political reasons. Now let’s move on to diseases that are embraced by mainstream medicine.
Hepatitis C
The earlier hep C treatments involved a combination of drugs usually involving interferons. Your bodily naturally produces interferons to fight viruses and there are many different types of interferons. The pharma industry figured out that interferons can be modified through pegylation. According to D E Baker:
Pegylation of the interferon increases the amount of time the interferon remains in the body by increasing the size of the interferon molecule . Increasing molecule size slows the absorption, prolongs the half-life, and decreases the rate of interferon clearance.
Pegylated interferons - PubMed.
Interferons can have unpleasant side effects but they have some effective against a broad range of viruses.
The ex Soviet bloc countries use a number of different interferon drugs that are not approved in the Western world (e.g. tilorone). Some of them cause your body to produce interferons. Others are low-cost interferon drugs that are much cheaper than pegylated interferons.
Pharma innovation
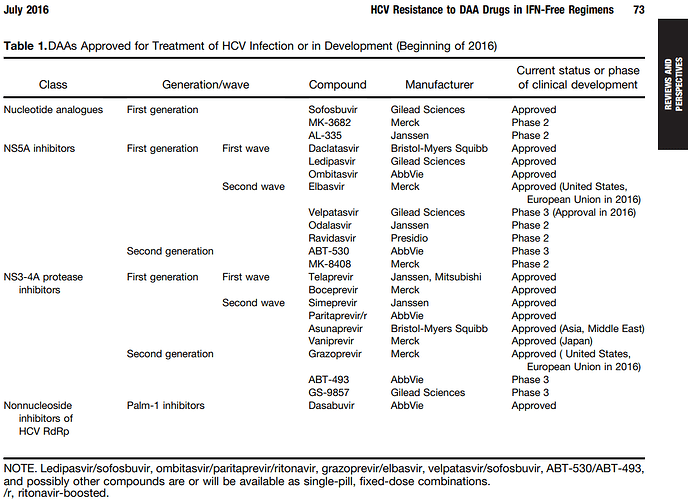
The pharmaceutical industry discovered new molecules that attack the Hep C virus at new angles.
When used in synergistic combinations, these drugs are highly effective at curing Hep C and eradicating it from the body (which didn’t happen that often with earlier treatments). Treatment sometimes only took 2 months instead of 2 years.
These drugs weren’t that profitable because cured patients don’t keep coming back for more, unlike Humira which does not cure disease (which was the best-selling drug in the world before the pandemic).
Hep C drugs for chronic illness
Sofosbuvir has been discussed on the subReddit r/CovidLongHaulers with a few people reporting success.
It turns out that the original anecdotes about sofosbuvir maybe weren’t that reliable as Warm_Camera_7052 (and his sibling) did not follow through and post updates about their sofosbuvir experience.
There is a little anecdotal evidence regarding tilorone.
Hip (ME/CFS patient) has posted about low-dose oral interferon alpha as one treatment that was successful in treating ME/CFS (search for ‘low-dose oral interferon alpha’ in the thread linked to from here).
Resistance
Unfortunately, in some patients, the virus will mutate/evolve and develop resistance against one of the drugs. That can allow the virus to persist in the patient. There are various strategies that try to prevent resistance from developing.
HIV
While treatment does not lead to a cure, treatment can suppress HIV to a very low level so that patients can enjoy fairly normal lives.
Drug resistance can be a problem and combinations of drugs are widely used.
HIV drugs for chronic illness
Tenofovir makes multiple appearances in Hip’s list of ME/CFS successes.
Various HIV drugs seem to have cured multiple sclerosis (though the response rate is likely very low). Search the slides here. Certain autoimmune diseases seem to be more common after the onset of chronic illness - see the Risk Factors survey data.
Maraviroc is technically a HIV drug; however, the theory behind using maraviroc for chronic illness doesn’t involve fighting pathogens or a virus like HIV. Data is available on leronlimab, a different CCR5 antagonist. See here.
Putting it together
The concept of synergy is an interesting one. Drug combinations are a cornerstone of treatment when it comes to curing tuberculosis and Hep C. Essential oils are naturally-existing cocktails of chemicals that plants use to fight microbes; the synergistic effects may be responsible for black seed oil being one of the top treatments according to survey data. However, the response rate on black seed oil is low so I don’t think that its synergy is that powerful. In practice, we don’t even know what we’re fighting so it would be difficult to figure out the proper synergistic combination to fight an unknown microbe. With enough experimentation, patients may be able to figure out synergistic combinations that wipe out their problem.
The concept of microbes developing drug resistance likely matters. However, I don’t think we can do much about it right now unless we detect infections that we already know how to treat.
Pulsing is interesting but not needed to fight chronic Lyme. It is not an effective strategy for viruses.
Lastly, some of the drugs have off-target effects on other microbes (e.g. HIV drugs that treat Hep B) and those are really interesting for chronic illness (because they may fight microbes that haven’t been discovered yet), especially when some HIV drugs have led to multiple sclerosis going into remission. Those drugs may (or may not) be useful in patients where everything else has failed. e.g. Emtricitabine / Tenofovir, interferons, tilorone (interferon inducer and antiviral), artemisinins, etc.