Dr. Steven Phillips developed chronic illness that left him unable to work and unable to care for himself. After successfully treating himself (it took 2 years), he started to specialize in treating other people like him (in the alternative self-pay system).
He believes that vector-borne illnesses from ticks, mosquitos, spiders, etc. are responsible for many chronic illnesses such as chronic Lyme, autoimmune disease, and some forms of dementia. As he became aware of Long COVID (and post-vax), he has since been changing his thinking on chronic illness. See his May 2022 Substack post and Mar 2023 interview.
One of the threads that runs through chronic illness is that many recoveries have been attributed to antimicrobial drugs.
- Multiple sclerosis - case reports of being cured with various HIV antivirals (see the slides in this video’s description)
- Chronic Lyme is from Lyme bacteria
- Post-vax and to a lesser extent Long COVID - 5 of the top 6 treatments have anti-microbial properties
- ME/CFS - Antimicrobials are common in Hip’s list of success stories, though other treatments frequently appear too. John Chia is a ME/CFS specialist who often treats patients with antimicrobials - see my previous profile on him.
Treatment approach
While Stephen Phillips briefly mentions various azole antifungals in his Dr Been interview, his website has no mention of the word “fluconazole”. However, he does mention that fluconazole is effective against Lyme bacteria:
and then in my practice i use a lot of non-antibiotic antimicrobials. Like people would be very surprised to hear that fluconazole which is an antifungal actually has number one activity against the lyme bacteria and number two activity against uh bartonella and number three activity against Leishmaniasis you know the tropical parasite Leishmaniasis.
So people tend to put these antimicrobials into these little boxes and say this is an antibiotic this is an antifungal this is anti-parasitic and when you think about just how intimately related life is on the planet these labels become so silly
I don’t believe that fluconazole is a popular Lyme treatment but there are scientific studies that support its use. Megan Weitner wrote about it in her 2016 thesis (see my summary / cheat sheet). Her research lab at the time published a paper related to her work. Schardt also has a case series on using fluconazole for Lyme neurooborreliosis.
And while the Megan Weitner / Ying Zhang / Jie Feng group likes drug combinations that include cephalosporin antibiotics, Stephen Phillips mentions why he doesn’t like cephalosporins:
(40:08) then another case an infectious doctor asked me to take over a patient and treat her with a cephalosporin which we don’t use in the practice because of the high rates of C. Diff so we’re very very uh concerned and careful about the microbiome and you can use antimicrobial therapies that do not disturb it very much and i just wanted to make that point clear […]
His approach to treating Lyme is certainly quite different than other practitioners. Unfortunately, he doesn’t seem to have published much on his unique approach despite writing a book called Chronic. His Dr Been interview largely skips over the intricacies of treating any vector-borne illness.
His approach seems to consist of a lot of trial and error, trying various treatments to figure out what works. His experience in many treatments failing likely explains why he thinks that there are many different infectious agents that lead to chronic illness.
He does order tests for chronic infections based on the patient’s history and financial situation. However, he believes that tests will miss a lot of chronic infections.
Story
His story at the 4:31 mark of his interview with Dr. Been:
I got spider bites and i didn’t think anything of it because we’re not thought to treat spider bites with antibiotics or worry about them in any way
Within a couple of months I had a rapidly progressive arthritis with my spine and all over. I ended up getting systemically ill, getting very very anemic
My hematocrit was 25
My weight plummeted
I lost 50 pounds in a matter of months. I had a large spleen. I started getting fevers 102 every night and within six months I couldn’t take a single step on my own. I couldn’t walk for the following two years I gave up my practice I was completely bed bound everyone thought I was gonna die myself included and I required 24-hour home care
Differences between Lyme and Long COVID and post-vax
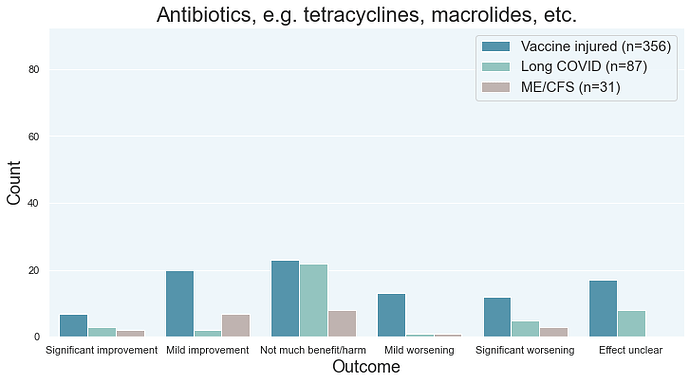
In the chart below, just focus on the “significant improvement” and “significant worsening” bars in the diagram below. If you have LC, post-vax, or ME/CFS, you’re more likely to experience significant worsening than significant improvement from antibiotics.
Antibiotics were rated very poorly by surveyees. Grouped together, that class of drugs was fighting it out for last place alongside exercise, SSRIs, TCAs, and psych drugs. They’re among the riskiest drugs that you can try.
This suggests to me that chronic Lyme is not occurring in the majority of long haulers. If there was chronic Lyme, antibiotics would perform reasonably well as they can be mediocre to excellent in treating Lyme. Antibiotics are regularly used to treat Lyme, though research suggests that some antibiotics like cephalosporins are better than others.
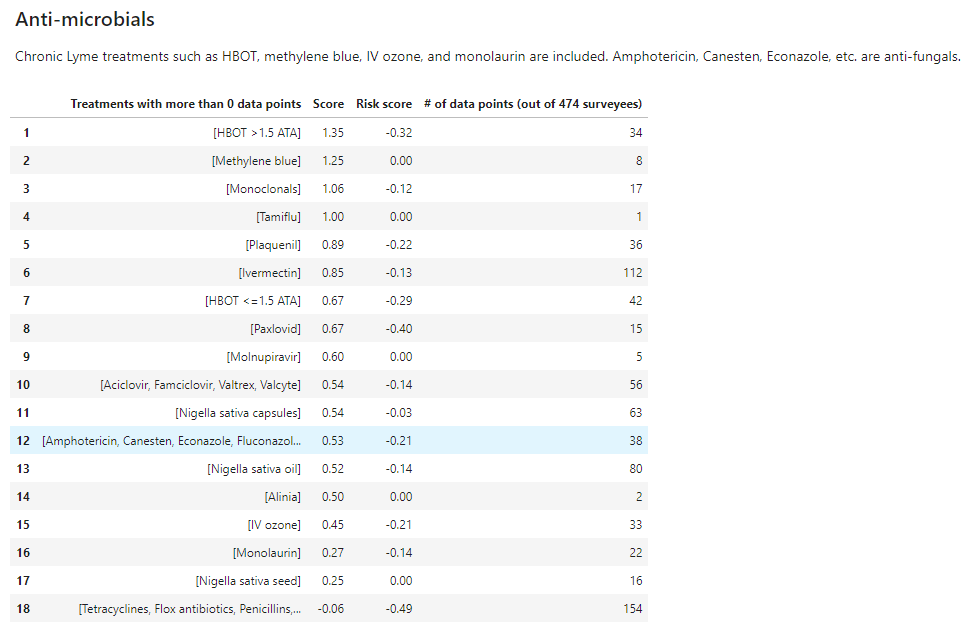
And here’s some data as to how fluconazole and other antifungals stack up against other anti-microbials. In the Treatment Outcomes survey data, no long haulers recovered on antifungals while 1 or more recoveries were seen with ivermectin, HCQ, high ATA HBOT, and black seed oil (nigella sativa oil). Statins were not included, though one can argue that they have antimicrobial properties.
- NOTE: The methodology is not very good because many responses come from people who didn’t recover. Their responses are likely less reliable (on average) because they haven’t experienced dramatic recovery.
While Steven Phillips really likes monolaurin, it is further down the list.
Recap
Phillips gives out very little treatment information. He kind of glosses over his highly unusual approach to treating Lyme. However, his main message is that doctors and patients should pay more attention to vector-borne illnesses as a cause of chronic illness.
Unfortunately he doesn’t try to explain how to treat these vector-borne illnesses. His unique approach is very nuanced and I couldn’t find much public information on it.
His story is interesting as he’s had real success in treating a chronic illness patient (himself) and he’s one of the people who believes that persistent/chronic infections are a cause of chronic illness.