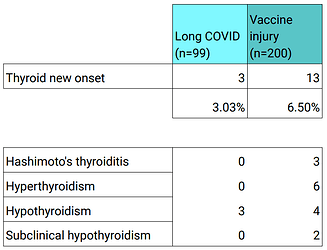
Data from the Risk Factors Survey shows a high rate of newly-diagnosed thyroid conditions in long haulers. The rate of new thyroid diagnoses was 3.0% in surveyees with Long COVID and 6.5% in post vax surveyees.
See slide 39 onwards.
A paper from a single center in Milan (DOI:10.1530/endoabs.81.P200) had somewhat similar findings - the authors found high rates of subacute thyroiditis and Grave’s disease in the newly vaccinated.
Symptoms of thyroid disorders
Hyperthyroidism, or an overly active thyroid
Common symptoms include:
- Anxiety
- Difficulty concentrating
- Fatigue
- Frequent bowel movements
- Goiter (visibly enlarged thyroid gland) or thyroid nodules
- Hair loss
- Hand tremor
- Heat intolerance
- Increased appetite
- Increased sweating
- Irregular menstrual periods in women
- Nail changes (thickness or flaking)
- Nervousness
- Pounding or racing heart beat (palpitations)
- Restlessness
- Sleep problems
- Weight loss (or weight gain, in some cases)
See that UPenn website for a list of other common symptoms. They show an illustration of what a swollen and abnormal thyroid gland looks like:
If your neck is swollen, you should (probably) talk to a doctor to figure out if your thyroid is swollen, your lymph nodes are swollen, etc.
The opposite of hyperthroidism is hypothyroidism, where your thyroid isn’t active enough. Symptoms:
Early symptoms:
- Hard stools or constipation
- Feeling cold (wearing a sweater when others are wearing a t-shirt)
- Fatigue or feeling slowed down
- Heavier and irregular menstrual periods
- Joint or muscle pain
- Paleness or dry skin
- Sadness or depression
- Thin, brittle hair or fingernails
- Weakness
- Weight gain
Late symptoms, if untreated:
- Decreased taste and smell
- Hoarseness
- Puffy face, hands, and feet
- Slow speech
- Thickening of the skin
- Thinning of eyebrows
- Low body temperature
- Slow heart rate
A few people can also flip between an overactive and underactive thyroid. It’s discussed in scientific papers like this one:
“Spontaneously oscillating thyroid function in Graves’ disease is a rare phenomenon.”
Alternating hyperthyroidism and hypothyroidism in Graves’ disease
Alternating hyperthyroidism and hypothyroidism in Graves’ disease - PMC
You would want to get your thyroid checked on multiple occasions if that is the case.
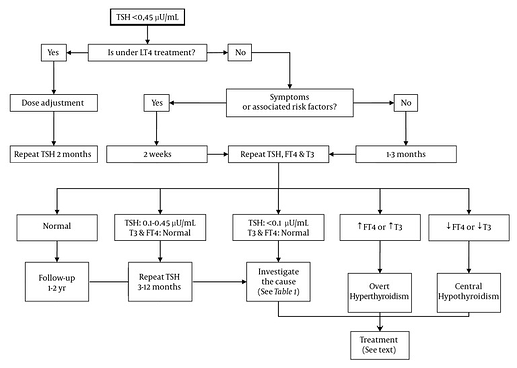
There are different markers of thyroid function that can be measured, but TSH (Thyroid Stimulating Hormone) level is the bread and butter. Doctors will have different preferences as to ordering additional tests on top of TSH - Free T3, Free T4, T3, T4, etc.
→ There are also various tests for antibodies against thyroid-related proteins (e.g. anti-TPO). They can help detect thyroid issues that may be autoimmune-related.
Subclinical (‘borderline’) hyper/hypothyroidism
Some doctors believe in this and others don’t. So let me explain what this is with an analogy to obesity. Some people are clearly obese and others aren’t. There’s also a grey area where people are on their way to being obese. The same applies for overactive thyroids and underactive thyroids. You can be part of the way there.
The controversy exists because some doctors believe that hypothyroidism is an “all or nothing” condition- you either have it or you don’t. It’s like you either have a missing tooth or you don’t. You either have the flu or you don’t. There’s no middle ground.
Let’s suppose that you believe that subclinical hypothyroidism is real. Here’s what the scientific literature is saying about it:
Subclinical hypothyroidism (SCH), also called mild thyroid failure, is diagnosed when peripheral thyroid hormone levels are within normal reference laboratory range but serum thyroid-stimulating hormone (TSH) levels are mildly elevated. This condition occurs in 3% to 8% of the general population. It is more common in women than men, and its prevalence increases with age. Of patients with SCH, 80% have a serum TSH of less than 10 mIU/L. The most important implication of SCH is high likelihood of progression to clinical hypothyroidism. The possibility that it is a cardiovascular risk factor has been a subject of debate.
Subclinical Hypothyroidism: An Update for Primary Care Physicians - PMC
So you can look at your TSH test result to see if it’s in the 5-10 mIU/L range (or higher). If it’s mildly elevated, then you may or may not have subclinical hypothyroidism.
Before recommending routine screening of the general population, large-scale randomized trials are needed to prove that treatment will improve quality of life in otherwise healthy patients who have the mildly elevated TSH level (5-10 mIU/L) typical of most SCH cases.
Subclinical hyperthyroidism can occur when your TSH is at the low end for your age, e.g. below 0.4 mIU/L or0.45.
See Management of Subclinical Hyperthyroidism - PMC for more information.
The bottom line
There is treatment for hypo and hyperthyroidism that can improve your quality of life. You may also get a diagnosis of an autoimmune disease like Grave’s or Hashimoto’s.
It’s probably worth getting your thyroid checked out if you have the symptoms. I hope that helps.