Summary
A company called MicroB-plex makes a test that measures antibody-secreting cells (ASCs). They isolate those cells, grow them in their special media (special sauce that helps the cell multiply), and then measure the antibodies produced by the ASCs. This test allows them to better measure if there is an active infection that is provoking the body into making ASCs to fight off an infection.
In my opinion, this test is not particular promising. We already know that targeting a latent SARS2 infection doesn’t work because Long COVID patients have tried Paxlovid, ivermectin, hydroxychloroquine, famotidine, most drugs listed at c19early.com, etc. In the unlikely event that SARS2 persistence truly is the cause of Long COVID, we simply don’t have the right drug yet. It’s possible that other reactivated infections are causing Long COVID but I don’t see this test as being helpful right now- it’s not there yet.
Long-winded explanation
The manufacturer provides some more nerdy details about their test:
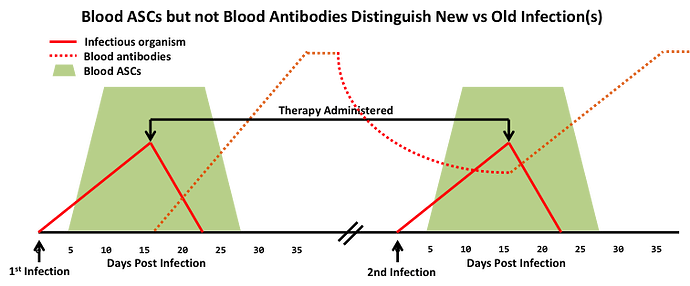
The disappearance of pathogen-specific ASCs from blood circulation is a definitive indication that the pathogen is no longer present, i.e., the infection has been resolved. Importantly, unlike pathogen-specific blood antibodies that are detectable for long periods, i.e., years in many cases, after elimination of the infecting pathogen, the presence of pathogen-specific blood ASCs distinguishes a current active infection from a prior infection with the same pathogen as illustrated in the accompanying figure.
Source: microbplex.com/technology/
People from the company were involved in a Long COVID study that has been published as a pre-print:
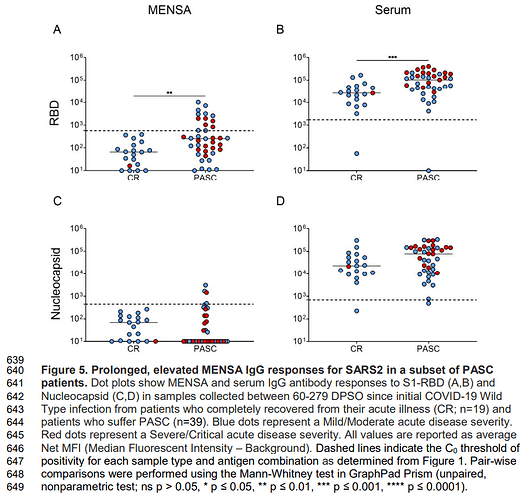
I would be very cautious about the reported results due to the problems inherent with measuring antibodies. Antibodies will stick to things that somewhat resemble spike protein but aren’t spike protein. This test may be finding ASCs that are targeting something other than SARS2 spike protein. That was a huge problem for another group that measures trace amount of spike protein in the blood - see this post on the Swank and colleagues study.
A second problem is that many patients don’t produce antibodies against the Nucleocapsid (N) protein of SARS2. Those people won’t test positive (for nucleocapsid antibodies) even when they are fighting off an active infection. Yet this research group is claiming that almost all patients do- that is very very suspicious.
MENSA = MicroB-plex’s test
Serum = looking for IgG antibodies in blood/serum
There’s something wonky going on with their methodology.
Also note that there is an incentive for the authors to make their research sexy, so it’s not unusual for researchers to bend the data to support some sexy claims like finding the cause of Long COVID.
The data is… meh
For the sake of argument, let’s pretend that there aren’t issues with the methodology.
Most people did not test positive on MicroB-plex’s MENSA test:
- In the 39 PASC (Long COVID) patients, 33% still had positive MENSA for spike RBD (after 60 DPSO) compared to none in the control group of COVID recovered patients.
- Only 10% of the PASC patients has a positive MENSA for nucleocapsid (see Figure 5C earlier in this post) compared to none in the control group.
- The control group of COVID recovered patients was only 19 people.
The research group also looked at EBV, CMV, and HSV2. Those are all active latent infections that occur in healthy people at lower rates.
The bottom line
This may be a bad tool for understanding latent infections. Next generation sequencing (NGS) will likely see more clinical use for finding active infections; it likely has fewer false positives than MENSA. The problem with NGS is that the Western medical system isn’t setup to make money from it. No money means that there won’t be much research interest in applying it for Long COVID.